

Even with a lack of crucial supplies, the Los Angeles Jewish Home takes early action to protect residents as 3 contract coronavirus; helps similar facilities cope
By NOAM HAYKEEN Today, 4:48 pm
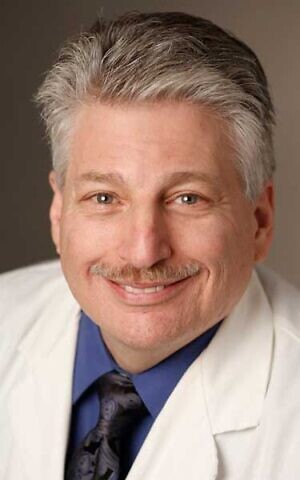
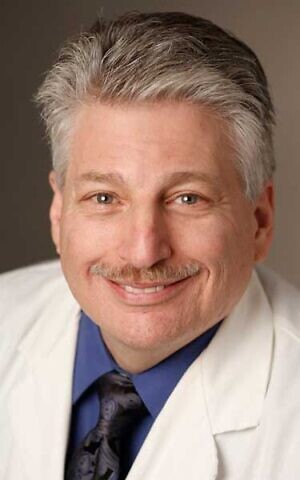
LOS ANGELES — Just prior to a mid-March management meeting at the Los Angeles Jewish Home, Chief Medical Officer Dr. Noah Marco received notice that a resident at the sheltered living facility had tested positive for COVID-19.
With an average age of 90, LAJH’s residents are part of the group that is “most susceptible and vulnerable to serious complications from this virus,” Marco said.
Marco scrambled to take the next steps. He notified LAJH’s leaders and the patient’s family and roommate. LAJH began creating a public communications operation to ensure its community was kept updated on how the organization intended to respond.
The infected resident ultimately recovered and returned to LAJH. However, two other residents have tested positive for COVID-19 since then. One died late last month. Four staff members at LAJH have also tested positive.


However, even with its recent coronavirus cases, the organization is facing a lack of testing resources because “the testing process [in the US] is incredibly resource-limited,” Marco told The Times of Israel. LAJH began testing its residents and staff on April 1. As of April 10, just five percent of residents and 10% of staff at LAJH had been tested for COVID-19.
The shortage of testing mirrors a countrywide predicament. According to David Eisenman, professor of medicine and public health at the University of California, Los Angeles, “a combination of bureaucracy, regulations, and lack of competent governance led the FDA and the CDC to the point where they were flatfooted when the virus landed here.”
To mitigate the impact of COVID-19, LAJH began implementing policies on March 4, the same day California experienced its first coronavirus death. It began screening all visitors and staff with temperature checks before they could enter its facilities. The normally activity-filled senior center suspended group activities that include people from the outside community.
As the health crisis worsened and members within LAJH were impacted, the institution began applying stricter measures. LAJH created isolation rooms for residents who test positive for COVID-19 to reduce the transmission of the virus. LAJH also set up a special wing for residents coming back from the hospital or the outside community to be placed in for 14 days.
On March 29, Marco connected with Los Angeles Mayor Eric Garcetti, and LAJH was chosen as a distribution hub of testing for the Los Angeles senior community. The organization became part of a citywide effort to increase testing initiated by Garcetti, Deputy Mayor Jeff Gorell, and the UPS delivery service.
But LAJH received only 500 test kits for its population of 1,100 residents and 1,300 staff. With the obligation to distribute the test kits to two other facilities, only a small fraction of the community has been tested. LAJH also created a list of 10 additional organizations that are interested in receiving future test kits.
A nationwide predicament
The senior living center created a testing unit for residents inside its facilities. Among the portion of the staff that was tested, some were tested at the center and others offsite. Once tested at LAJH, individuals wait two to four days to receive their test results. Residents and staff who were ill or identified as having a high risk of exposure were prioritized.
LAJH does not know when new test kits will be provided. Although the original plan was for the organization to obtain new tests on an ongoing basis, “bureaucracy and process issues prevented that from happening,” Marco said.
According to UCLA’s Eisenman, “Approved lab kits did not make it out to local testing sites fast enough. It was impossible to scale up so quickly for something that should have been scaled up in the weeks and months before COVID-19 arrived.”
Without testing, residents must be isolated from each other at all times, Eisenman explained. “This creates terrible loneliness, anxiety [and] depression,” he added. “This can hasten other illnesses and lead to other poor outcomes.” Eisenman expects this reality will lead to a decline in emotional and cognitive health.
Up to 25% of infected individuals remain asymptomatic, according to the director of the Centers for Disease Control and Prevention, Dr. Robert Redfield, which means workers who feel fine may indeed be spreading the illness.
“The testing for both staff and seniors at senior living facilities is very critical to prevent potential outbreak of COVID-19 in this vulnerable population,” said UCLA professor of epidemiology and medicine Zuo-Feng Zhang.
Please test our parents — and their caretakers
Mike Sirota, whose mother lives in the Eisenberg Village of LAJH, expressed worry about the limited government-provided testing resources.

“It worries me… [residents] might be infected, and they don’t know it. It would be good for them to know it, so they could prepare themselves for treatment,” Sirota said. “If the workers at the center could be tested, then we could inform people to not show up to work if they have the virus,” he added.
Efforts to combat COVID-19 have reshaped residents and family members’ lives. A few weeks ago, Rachel Kaufman and her family went to LAJH before Shabbat. Kaufman’s mother, Margarete, 77, lives at the Eisenberg Village of LAJH and has Parkinson’s disease. The family members stood six feet apart from each other and across the street from LAJH. Margarete was on the third floor as she watched her family through the window.
The family brought signs that read “We love you,” “Shabbat shalom,” and “Thank you to the nurses and staff.” They sang familiar Jewish songs such as “Gesher Tzar Me’od” and “Yedid Nefesh.”
“Seeing us is oxygen for her,” Kaufman’s father Joshua said. “It’s a tragedy that I have to be separated from my wife. She deserves all the honor. I owe everything to her.”
“Since then, we have been able to Skype,” said Rachel Kaufman. “We continue to sing. We see her lips moving, and her eyes perk up when she sees us. My dad usually blesses all of his children on Friday night, but before Passover, he said the blessings to my mom over Skype. We answered [by saying] ‘Amen.’”
Source: The Times of Israel





